Last year, the Centers for Medicare & Medicaid Services (CMS) finalized the CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F), a significant step toward improving healthcare efficiency, enhancing patient access to care, and reducing administrative burdens. Agadia shared various blog posts throughout the year to help health plans and PBMs navigate these upcoming changes, highlighting how our leading prior authorization solution, PAHub, can support compliance and streamline operations. Many of our customers have already begun implementing these adjustments and are well-prepared for the rule’s January 2026 effective date. Has your company taken the necessary steps to adapt? If not, here’s what to expect and how Agadia can help ensure a seamless transition.
Key Highlights of the Final Rule
The new CMS rule, effective January 2026, is designed to streamline prior authorization processes and enhance interoperability between payers and providers. Some of the most impactful provisions include:
- Faster Prior Authorization Decisions: Payers must respond to prior authorization requests within 72 hours for urgent requests and seven calendar days for standard requests—a significant improvement over existing timelines.
- Automated Prior Authorization via APIs: The rule mandates that impacted payers implement a Prior Authorization API, enabling providers to send and track requests electronically, reducing manual effort and delays.
- Greater Transparency in Decision-Making: Payers must publicly report prior authorization metrics and provide specific reasons for denials, fostering accountability and clarity.
- Enhanced Interoperability: Medicare Advantage, Medicaid, and CHIP payers are required to share patient data seamlessly using FHIR-based APIs, ensuring continuity of care and reducing redundant administrative work.
How Agadia Can Help
As a leader in prior authorization automation, Agadia’s PAHub solution is designed to align with the CMS mandates, ensuring Health Plans and PBMs stay compliant while enhancing efficiency.
Here are the CMS final rule provisions & PAHub’s key contributions to address these requirements:
CMS Final Rule Provisions & PAHub’s Key
Contributions to Address These Requirements


Patient Access API:
The rule mandates the implementation of an HL7® FHIR® Patient Access API, including information about prior authorizations, by January 1, 2027. To ensure transparency and patient understanding, impacted payers are required to report annual metrics on Patient Access API usage starting January 1, 2026.

Provider Access API:
To support care coordination and value-based payment models, impacted payers must implement and maintain a Provider Access API by January 1, 2027. This API facilitates the exchange of patient data, including individual claims, encounter data, and specified prior authorization information.

Payer-to-Payer API:
To enhance care continuity during payer transitions, impacted payers are obligated to implement and maintain a Payer-to-Payer API by January 1, 2027. This API enables the sharing of claims and encounter data, fostering seamless access to relevant patient information.

Prior Authorization API:
Impacted payers are required to establish and maintain a Prior Authorization API, ensuring standardized communication on covered items and services. The API must convey approval, denial, or requests for more information regarding prior authorization, with implementation starting January 1, 2027.

Prior Authorization Decision Timeframes
Impacted payers (excluding QHP issuers on the FFEs) are required to send prior authorization decisions within 72 hours for expedited (i.e., urgent) requests and seven calendar days for standard (i.e., non-urgent) requests.

Provider Notice, Including Denial Reason:
Beginning in 2026, impacted payers must specify the reason for PA denials, communicated through various methods like portal, fax, email, mail, or phone. This aims to enhance communication, transparency, and provider resubmission capabilities, excluding prior authorization decisions for drugs, with existing notice requirements for certain payers remaining unchanged.

Prior Authorization Metrics:
Impacted payers are required to publicly report certain PA metrics annually by posting them on their website. These operational or process-related policies are being finalized with a compliance date starting January 1, 2026, and the initial set of metrics must be reported by March 31, 2026.

Required Standards and Recommended
Implementation Guides (IGs) for APIs:


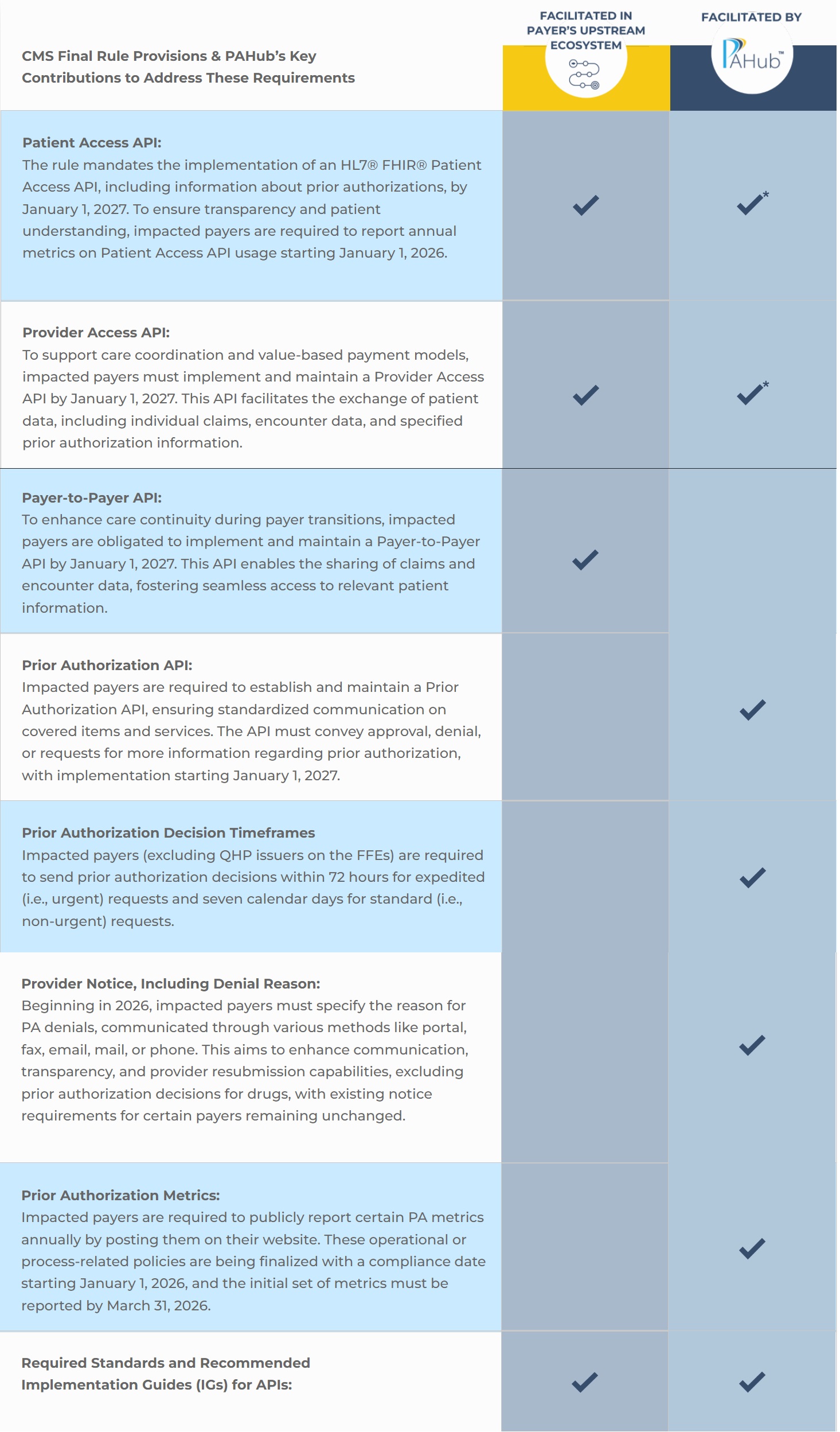
*This capability is on the PAHub release roadmap and will be in place prior to the CMS requirement deadline.
With the January 2026 deadline approaching, payers must act now to implement the necessary technological updates. Agadia is ready to support health plans in achieving compliance while optimizing operational efficiency.
Stay ahead of regulatory changes and schedule a demo today to learn how we can help you navigate the CMS Interoperability and Prior Authorization Final Rule with confidence.










