CMS Final Rule Provisions & PAHub’s Key
Contributions to Address These Requirements


Patient Access API:
The rule mandates the implementation of an HL7® FHIR® Patient Access API, including information about prior authorizations, by January 1, 2027. To ensure transparency and patient understanding, impacted payers are required to report annual metrics on Patient Access API usage starting January 1, 2026.

Provider Access API:
To support care coordination and value-based payment models, impacted payers must implement and maintain a Provider Access API by January 1, 2027. This API facilitates the exchange of patient data, including individual claims, encounter data, and specified prior authorization information.

Payer-to-Payer API:
To enhance care continuity during payer transitions, impacted payers are obligated to implement and maintain a Payer-to-Payer API by January 1, 2027. This API enables the sharing of claims and encounter data, fostering seamless access to relevant patient information.

Prior Authorization API:
Impacted payers are required to establish and maintain a Prior Authorization API, ensuring standardized communication on covered items and services. The API must convey approval, denial, or requests for more information regarding prior authorization, with implementation starting January 1, 2027.

Prior Authorization Decision Timeframes
Impacted payers (excluding QHP issuers on the FFEs) are required to send prior authorization decisions within 72 hours for expedited (i.e., urgent) requests and seven calendar days for standard (i.e., non-urgent) requests.

Provider Notice, Including Denial Reason:
Beginning in 2026, impacted payers must specify the reason for PA denials, communicated through various methods like portal, fax, email, mail, or phone. This aims to enhance communication, transparency, and provider resubmission capabilities, excluding prior authorization decisions for drugs, with existing notice requirements for certain payers remaining unchanged.

Prior Authorization Metrics:
Impacted payers are required to publicly report certain PA metrics annually by posting them on their website. These operational or process-related policies are being finalized with a compliance date starting January 1, 2026, and the initial set of metrics must be reported by March 31, 2026.

Required Standards and Recommended
Implementation Guides (IGs) for APIs:


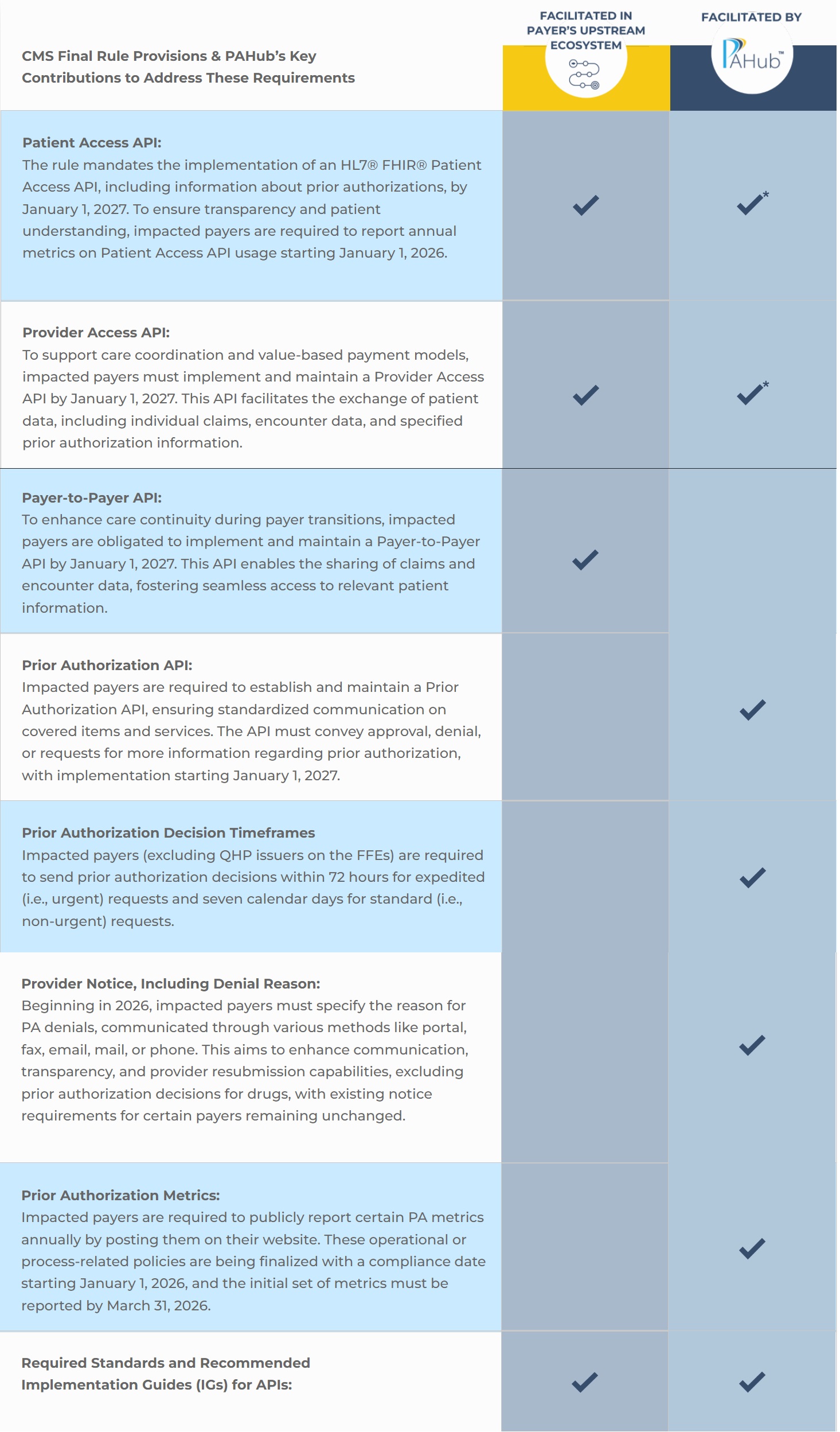
*This capability is on the PAHub release roadmap and will be in place prior to the CMS requirement deadline.
As healthcare organizations adapt to the evolving landscape shaped by CMS’s Prior Authorization Final Rule, PAHub stands out for its notable contributions. Focusing on meeting the stringent turn around timers, facilitating clinical criteria configuration, and advanced reporting capabilities, PAHub positions itself as a key player in enhancing compliance and efficiency. To explore how PAHub can support your organization in navigating the CMS final rule, consider scheduling a demo today and experience firsthand the benefits of a solution tailored to meet the unique challenges of prior authorization in healthcare.