Improve Clinical Efficiency & Compliance through
Prior Authorization Automation
with Agadia’s fully customizable web-based solution, PAHub


End to End management of Electronic Prior Authorizations
Delivering Electronic Prior Authorization Efficiency & Compliance
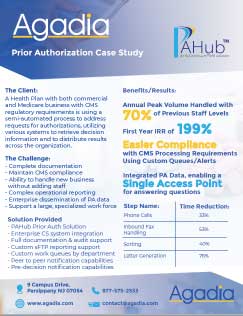
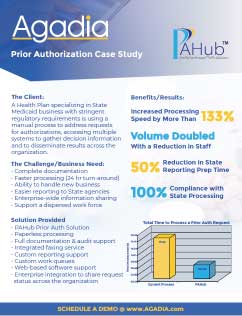
As Prior Authorization volumes continue to rise, and as specialty drugs create additional clinical complexities, Health Plans, Pharmacy Benefit Managers (PBMs) and Third-Party Administrators (TPAs) are challenged to adapt while maintaining or improving operational and clinical efficiencies. PAHub, is a HITRUST certified solution that puts the tools at your fingertips to streamline and control all clinical, compliance and administrative aspects of Prior Authorization at the point-of-care to improve compliance, reduce turn-around times and costs.
By leveraging the latest technologies for data mining, data analytics, content management and advanced decision support trees, PAHub, enables customers to automate the end-to-end prior authorization process.
All Lines of Business
Supported across all lines of business (commercial, Medicare, Medicaid, etc.)
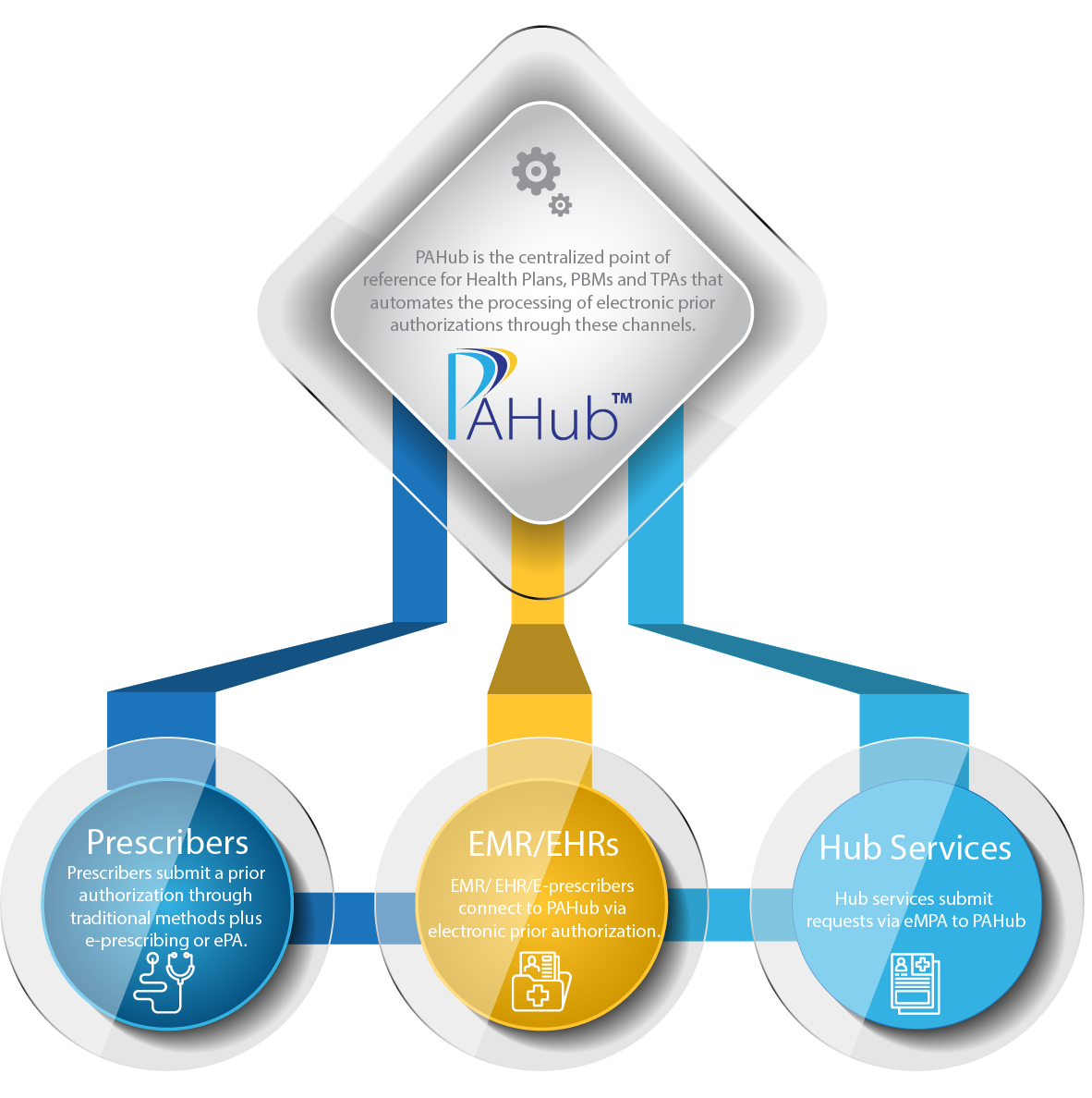
All Channels
Available across all channels (electronic prior authorization (ePA), phone, fax, web, e-prescribing, etc.)
All Healthcare Services
Applicable for all healthcare services, all benefit types (pharmacy & medical)
A Centralized Prior Authorization Solution
Continually Innovating to Meet Industry Needs
Addressing Electronic Prior Authorization for Drugs Under the Medical Benefit
With an influx of infused medications being administered in physician offices, prior authorizations for drugs billed under the medical benefit are presenting challenges across the industry. While there is an industry NCPDP SCRIPT standard for electronic prior authorization (ePA) for drugs billed under the pharmacy benefit, driving significant ePA volume, an industry standard does not currently exist for drugs under the medical benefit.

Agadia continues to innovate and has addressed these challenges by providing eMPA capabilities to reduce the prior authorization administrative burden through a more efficient channel that increases automation and improves turnaround times. Providers will benefit by quickly being informed whether the drug is under the pharmacy or medical benefit, allowing them to efficiently manage requests. Hub companies will experience improved efficiencies as well such as faster turnaround times for a prior authorization decision, improved patient speed to therapy and better adherence.
Leverage Advanced Technologies
Save Valuable Time & Resources with PAHub’s Auto-Decision
PAHub’s Auto-Decision rules engine increases automation be leveraging data mining techniques across enterprise systems data to electronically adjudicate prior authorization requests. Auto-Decision helps a customer to allocate staff to high-touch requests instead of requests that can be adjudicated automatically.
Engage Pharmacies, Members & Providers
In the Prior Authorization and Pre-Certification Process
PromptPA is a self-service, web based solution that enables our customers’ pharmacies, members and providers to request prior authorizations electronically, initiate renewals and check the status of requests using any web browser, reducing operational costs and call volume to Health Plans and Benefit Managers.

Quick Facts
Lives Covered Across Customer Base
Health Plan & Pharmacy Benefit Management (PBM) & Third-Party Administrator (TPA) Customers
Prior Authorizations Processed Annually
%
Electronic Prior Authorizations Processed
Phone
877-575-2533
contact@agadia.com
Location
9 Campus Drive, Parsippany NJ 07054
© 2025 Agadia Systems, Inc. All Rights Reserved.
Legal Information | Sitemap